Chronic lymphocytic leukaemia
Chronic lymphocytic leukaemia (CLL) is the most common type of leukaemia in Western countries.
The information provided on www.fcarreras.org is intended to support, not replace, the relationship that exists between patients/visitors to this website and their physician.
Information reviewed by Dr. Rocío Parody Porras, Doctor specialising in Haematology. Member of the Management of REDMO (Bone Marrow Donor Registry) and of the Foundation’s medical team. Barcelona Medical Association (Co. 35205)
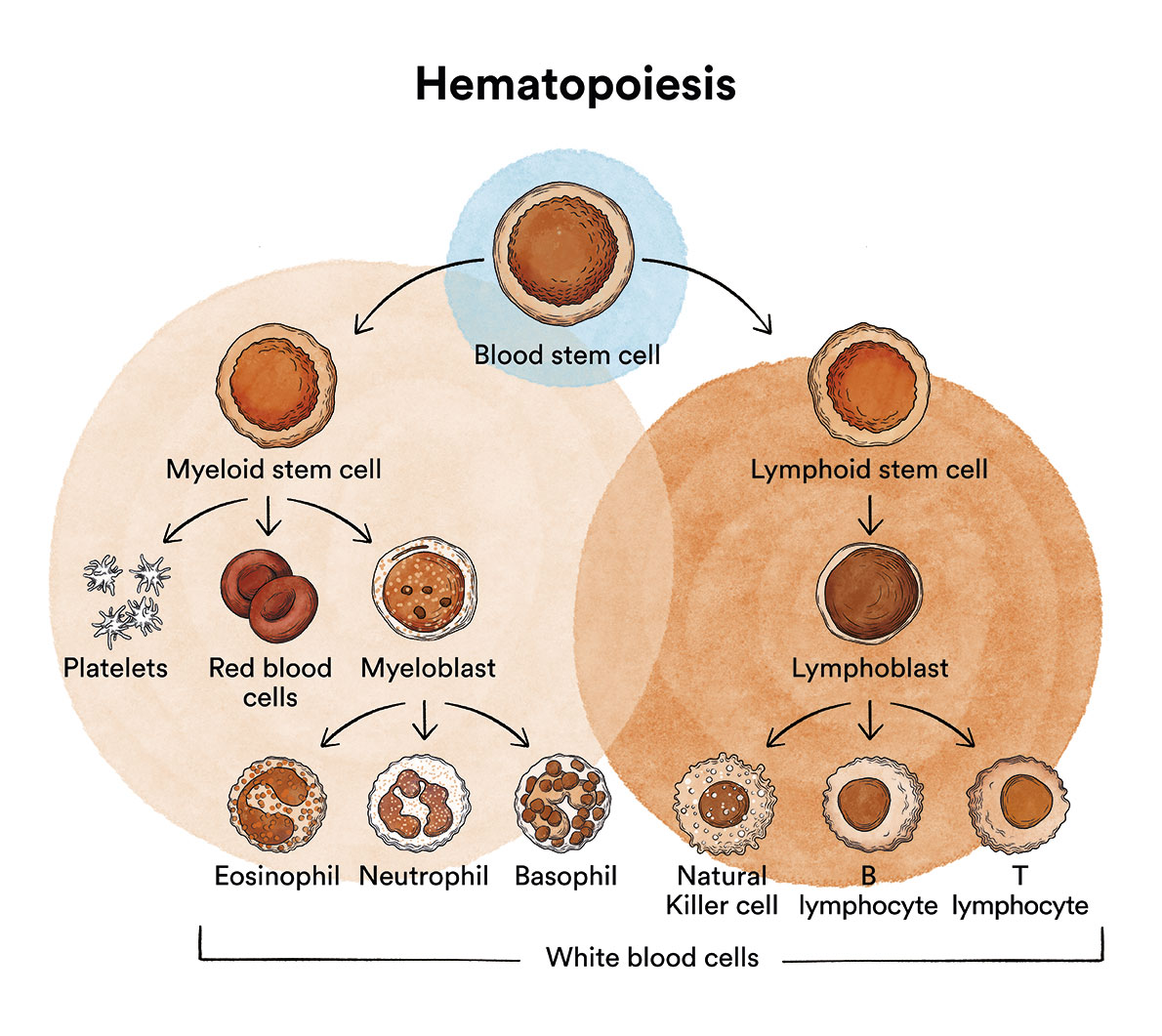
How does bone marrow work and what are the types of blood cells?
Chronic lymphocytic leukaemia (CLL) is a type of blood cell cancer that originates in the bone marrow. See section Leukaemia, bone marrow and blood cells.
What is chronic lymphocytic leukaemia and who does it affect?
Chronic lymphocytic leukaemia (also called chronic lymphoid leukaemia or CLL) is a type of chronic lymphoproliferative syndrome with leukaemic expression.
CLL is a blood cancer in which the bone marrow and organs of the lymphatic system produce an excess of B lymphocytes, a type of white blood cell. Under normal conditions, B and T lymphocytes are responsible for fighting infections, either by producing antibodies that attack harmful elements which invade or are produced in the body (B lymphocytes) or by attacking them directly (T lymphocytes).
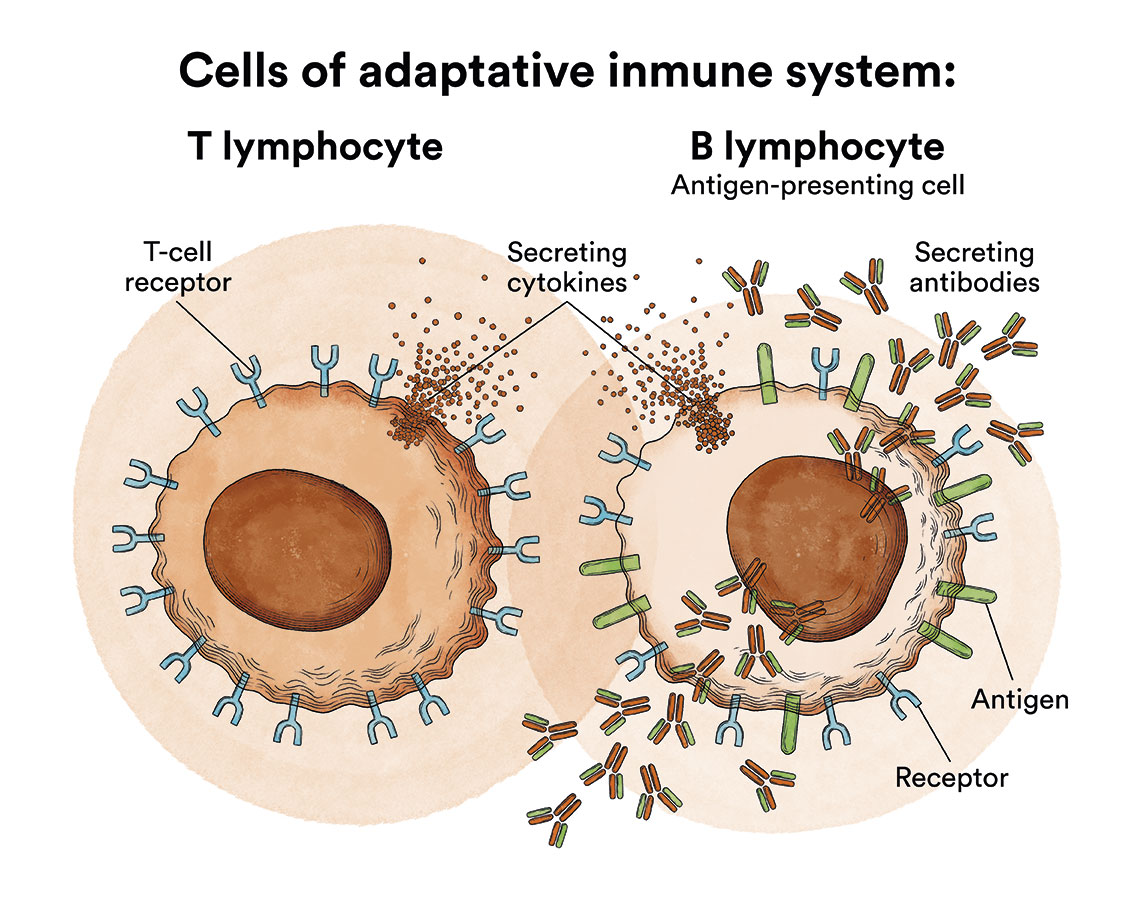
In CLL, B lymphocytes progressively infiltrate the bone marrow, lymphoid tissues (mainly lymph nodes and spleen) and other organs such as the liver. The clinical manifestations of the disease are a consequence of this infiltration, which displaces normal blood elements and prevents the proper functioning of the affected organs. In addition, the lymphocytes produced do not function properly and cannot fulfil their mission of defending the body.
CLL is the most common leukaemia in Western countries (20-40% of all leukaemias) and is rare in Eastern countries. In Spain, around 30 new cases per million inhabitants are diagnosed every year, which adds up to around 1,400 new cases every year in Spain.
CLL usually affects people over 60 years of age (median age of 70 years; only 20% are younger than 65 years), it is extremely rare in children, and it progresses very slowly. In many cases people with this disease do not develop symptoms for years, sometimes never.
What are the causes of chronic lymphocytic leukaemia?
It is not known why chronic lymphocytic leukaemia occurs, although it is the only leukaemia for which a higher incidence among family members has been reported (5%).
Chronic lymphocytic leukaemia, like other cancers, is not contagious.
What are the symptoms of chronic lymphocytic leukaemia?
In the early stages of chronic myeloid leukaemia, patients often do not feel any discomfort. The most frequent form of presentation of this disease is the chance finding of an analytical abnormality. In more than 80% of patients, CLL is diagnosed by a routine blood test or by chance as they are usually completely asymptomatic.
In other cases, the main symptoms may be asthenia, adenopathy (enlarged lymph nodes) and recurrent infections. Splenomegaly (swelling of the spleen) or hepatomegaly (enlargement of the liver) are not uncommon and can cause abdominal discomfort. In contrast to lymphomas, fever, night sweats and weight loss are infrequent (10%).
How is chronic lymphocytic leukaemia diagnosed?
To establish a diagnosis of CLL, a sustained blood lymphocytosis of ≥5 x 109 /l is required, together with a compatible morphological and immunophenotypic study, as well as cytogenetic and molecular studies to complement the diagnosis. Spinal cord examination with aspirate and biopsy (obtaining a cylinder of bone from the hip), once a conventional examination, is now often limited to patients under 70 years of age who require treatment. Similarly, it is not essential to biopsy one of the affected lymph nodes, unless transformation of CLL to Richter’s syndrome, a rare condition in which chronic lymphocytic leukaemia (CLL) develops into a fast-growing type of lymphoma, is suspected. The lymph node territories that are affected are also often studied using imaging techniques (especially computed axial tomography, known as CT or scanning).
In Europe it is customary to use the Binet classification to characterise CLL. Three distinct stages are differentiated, depending on the number of lymph tissue groups involved (neck lymph nodes, groin lymph nodes, axillary lymph nodes, spleen and liver) and whether or not the patient has anaemia (insufficient red blood cells) or thrombocytopaenia (insufficient platelets).
- Binet stage A: less than three enlarged lymphoid areas, no anaemia or thrombocytopaenia.
- Binet stage B: three or more enlarged lymphoid areas, no anaemia or thrombocytopaenia.
- Binet stage C: anaemia and/or thrombocytopaenia.
In the United States, it is customary to establish this staging using the Rai system, which ranges from 0 (lymphocytosis only), 1 (lymphocytosis in the aforementioned territories), 2 (if spleen and/or liver are affected), 3 (presence of anaemia due to marrow infiltration) and 4 (presence of thrombocytopaenia due to marrow infiltration). Binet and Rai stages A and 0, respectively, would be low risk, B and 1-2 would be intermediate risk and C and 3-4 would be high risk.
What is the treatment for chronic lymphocytic leukaemia?
Patients with early stage CLL (low risk) usually do not require treatment for years and can lead a normal life, except for the periodic check-ups they are obliged to undergo to monitor whether the disease progresses or remains stable. Quite often, living with a disease that requires untreated surveillance can be emotionally challenging for many patients, hence it is critical that they establish communication with their doctor.
The criteria for initiating treatment are the presence of:
- Very obvious systemic symptoms (fever, sweating, weight loss).
- The criteria for initiating treatment are the presence of:
- Very obvious systemic symptoms (fever, sweating, weight loss).
- Enlarged lymph nodes or enlarged spleen causing discomfort to the patient.
- Recurrent infections.
- Progressive increase of anaemia and/or thrombocytopaenia.
- Very fast lymphocyte doubling time (a lymphocyte count that has doubled in less than 6 months).
- Autoimmune complications (anaemia and/or thrombocytopaenia) that do not respond to corticosteroid treatment.
Very high lymphocyte counts alone are not a criterion for initiating treatment.
There are several options in terms of therapeutic alternatives: Treatments based on chemoimmunotherapy (point 1) and targeted treatments
- Treatment based on chemo–immunotherapy: combining fludarabine, associated with cyclophosphamide and Rituximab (monoclonal antibody targeting CD20, a marker present on lymphocytes). This treatment would be especially indicated for young patients. In patients over 65 years of age, the combination of bendamustine and rituximab is usually prescribed and is better tolerated. In patients with comorbidities, another option is chlorambuzil and obinotuzumab, another anti-CD20 monoclonal antibody.
- Treatments targeting specific molecules:
- Burton tyrosine kinase inhibitors such as ibrutinib or acalabrutinib, which can be combined with rituximab. Of choice for patients with TP53 alteration.
- BCL2 inhibitors such as venetoclax in monotherapy although it has recently been approved for use with obinotuzumab, another anti-CD20 monoclonal antibody. Indicated in patients where ibrutinib is contraindicated.
- Idelalisib (another type-specific kinase inhibitor) in combination with rituximab, approved for a CLL patient who has received at least one prior treatment, or as first-line treatment in the presence of 17p deletion or TP53 mutation in patients for which there is no other suitable treatment.
The choice of strategy will therefore depend on the availability of therapies, the patient’s age and tolerance, and the presence of high-risk factors such as TP53 and 17p mutations.
We must also be taken into consideration support treatment, given that it is a chronic disease and involves a certain degree of alteration of the immune system that prevents us from infections, and it may be necessary to use prophylactic antibiotic treatment (such as cotrimoxazole) or sometimes support with immunoglobulins, along with the treatment.
These therapies, which are generally well tolerated, are very effective and sometimes lead to molecular remission of the disease, a situation in which it is not possible to detect the disease even with the most sophisticated laboratory techniques. Despite this, none of these treatments can cure CLL, although the achieved remissions can be sustained for years.
Unlike other leukaemias, CLL is not usually treated with haematopoietic stem cell transplantation due to the advanced age of most patients. However, young patients with aggressive CLL can benefit from this therapeutic measure if they have a histocompatible donor, as this is the only therapy that can cure the disease.
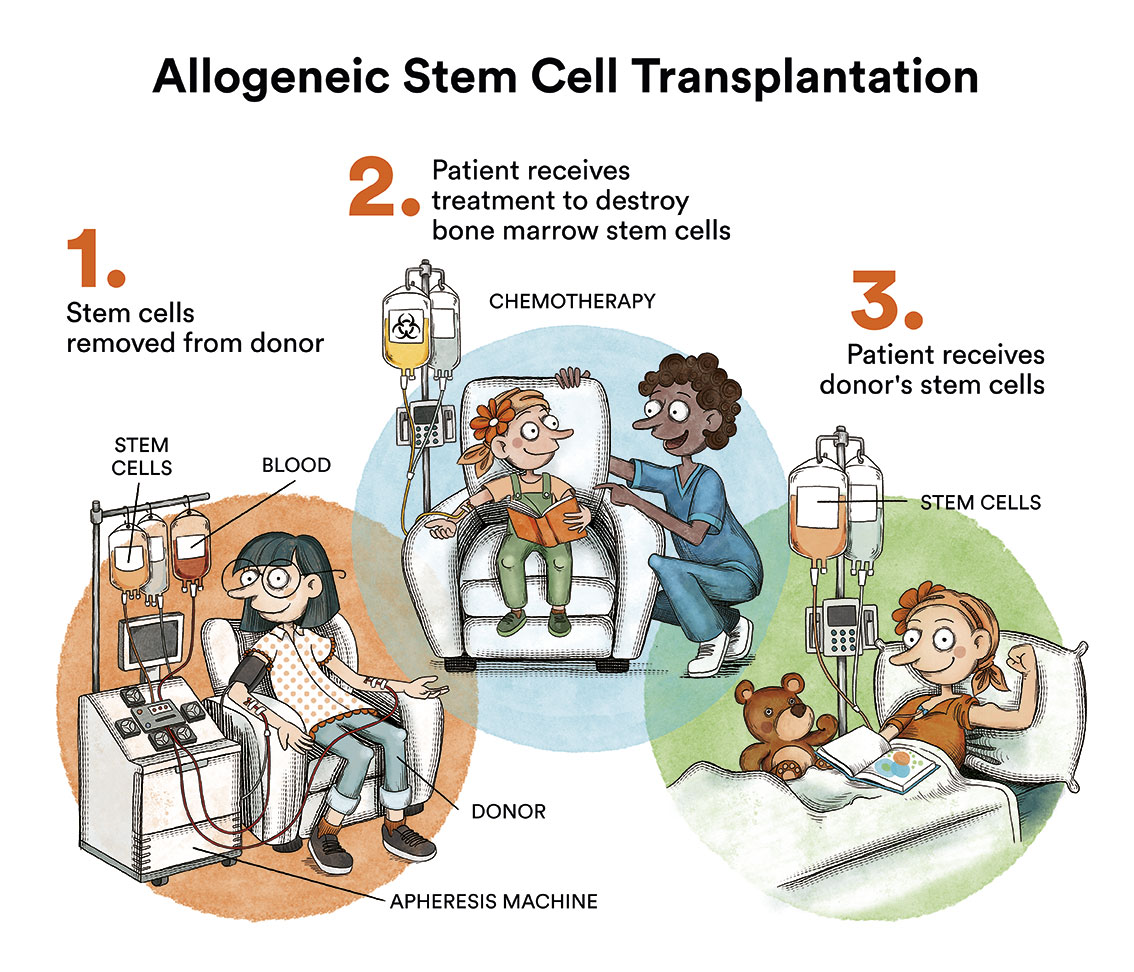
Autologous haematopoietic stem cell transplantation, although used for years to prolong the duration of remission, has been virtually abandoned as it is never curative and the availability of the new therapeutic regimens mentioned above.
Patients who have undergone a transformation to Richter’s syndrome should be treated as an aggressive lymphoma (see chapter on non-Hodgkin’s lymphoma).
What is the prognosis for patients with chronic lymphocytic leukaemia?
The prognosis of a patient with CLL is highly variable depending on the presence or absence of a number of prognostic factors, such as: the stage of the disease, the doubling time of the lymphocyte count, the elevation of beta2-microglobulin in the blood, the presence of certain cytogenetic alterations (trisomy 12 or deletions of chromosome 11 or 17), the increase of certain serum markers such as the expression of ZAP-70 or CD38 proteins, the presence of TP53 mutation, and the mutational status in the variable region of the immunoglobulin gene. For example, patients with mutations in the variable region of the immunoglobulin gene have a better prognosis as they tend to progress very slowly, do not usually require treatment, and can live for many years.
With the new therapies approved for CLL (ibrutinib and similar, and BCL2 inhibitors such as venetoclax) the prognosis for patients which was traditionally much poorer has greatly improved, although there are certain subgroups (such as those with the TP53 mutation and/or deletion of chromosome 17) who continue to have a poor response to treatment.
5-10% of CLL patients progress to an aggressive variety of lymphoma, called Richter’s syndrome, which requires intensive chemotherapy treatment.
A small percentage of patients (5%) experience (before or after CLL diagnosis) second malignancies (skin, digestive tract and lung).
Links of interest concerning medical issues relating to chronic lymphocytic leukaemia
- Chronic lymphocytic leukaemia (CLL). Cancer Research UK
- What Is Chronic Lymphocytic Leukemia?. American Cancer Society
- Chronic lymphocytic leukaemia (CLL). Blood Cancer UK
- Chronic lymphocytic leukemia (CLL). Leukemia & Lymphoma Society
- Chronic lymphocytic leukaemia (CLL). Macmillan Cancer Support
Links of interest on other topics related to chronic lymphocytic leukaemia
TESTIMONIAL MATERIALS
You can order the booklets in paper format for free delivery in Spain by e-mail: imparables@fcarreras.es
BONE MARROW TRANSPLANT
- Bone Marrow Transplant Guide. Josep Carreras Foundation (content in Spanish)
- What is HLA and how does it work? Josep Carreras Foundation (content in Spanish)
- Graft-versus-Host Disease. Josep Carreras Foundation (content in Spanish)
- History of Bone Marrow Transplantation. Josep Carreras Foundation (content in Spanish)
- How is the search for an anonymous donor conducted? Josep Carreras Foundation (content in Spanish)
FOOD
- How to maintain a healthy diet during treatment? Josep Carreras Foundation (content in Spanish)
- Nutrition guide. Leukemia & Lymphoma Society
OTHER
- Ideas on what to take with me to the isolation chamber. Josep Carreras Leukaemia Foundation (content in Spanish)
- Travel tips for people with cancer. Josep Carreras Leukaemia Foundation (content in Spanish)
- Physiotherapy manual for haematological and transplant patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Prevention and treatment of oral mucositis. Josep Carreras Leukaemia Foundation (content in Spanish)
- Oral hygiene in oncohaematological patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Fertility manual: Suffering from blood cancer and becoming a parent. Josep Carreras Leukaemia Foundation (content in Spanish)
- Skin care in the oncohaematological patient. Josep Carreras Leukaemia Foundation (content in Spanish)
- Aesthetic Oncology Manual. Josep Carreras Leukaemia Foundation (content in Spanish)
- Leukaemia and sexuality. Josep Carreras Leukaemia Foundation (content in Spanish)
- 7 ways to wear a scarf. Josep Carreras Leukaemia Foundation (content in Spanish)
Links of interest: local/provincial or state entities that can provide you with resources and services specialised in leukaemia or cancer patients:
In Spain there is a large network of associations for haematological cancer patients that, in many cases, can inform you, advise you and even carry out certain procedures. These are the contacts of some of them by Autonomous Communities:
All these organisations are external to the Josep Carreras Foundation.
STATE
- AMILO (Asociación Española de Amiloidosis)
- CEMMP (Comunidad Española de Pacientes de Mieloma Múltiple) Comunidad Española de Pacientes con Mieloma Múltiple | CEMMP (comunidadmielomamultiple.com)
- AEAL (ASOCIACIÓN ESPAÑOLA DE AFECTADOS POR LINFOMA, MIELOMA y LEUCEMIA)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact with the nearest branch or call 900 100 036 (24h).
- AELCLES (Agrupación Española contra la Leucemia y Enfermedades de la Sangre)
- CEMMP (Comunidad Española de Pacientes de Mieloma Múltiple)
- Josep Carreras Leukaemia Foundation
- FUNDACIÓN SANDRA IBARRA
- GEPAC (GRUPO ESPAÑOL DE PACIENTES CON CÁNCER)
- MPN España (Asociación de Afectados Por Neoplasias Mieloproliferativas Crónicas)
ANDALUCÍA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ALUSVI (ASOCIACIÓN LUCHA Y SONRÍE POR LA VIDA). Sevilla
- APOLEU (ASOCIACIÓN DE APOYO A PACIENTES Y FAMILIARES DE LEUCEMIA). Cádiz
ARAGÓN
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASPHER (ASOCIACIÓN DE PACIENTES DE ENFERMEDADES HEMATOLÓGICAS RARAS DE ARAGÓN)
- DONA MÉDULA ARAGÓN
ASTURIAS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASTHEHA (ASOCIACIÓN DE TRASPLANTADOS HEMATOPOYÉTICOS Y ENFERMOS HEMATOLÓGICOS DE ASTURIAS)
CANTABRIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LA MANCHA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LEÓN
- ABACES (ASOCIACIÓN BERCIANA DE AYUDA CONTRA LAS ENFERMEDADES DE LA SANGRE)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ALCLES (ASOCIACIÓN LEONESA CON LAS ENFERMEDADES DE LA SANGRE). León.
- ASCOL (ASOCIACIÓN CONTRA LA LEUCEMIA Y ENFERMEDADES DE LA SANGRE). Salamanca.
CATALUÑA
- ASSOCIACIÓ FÈNIX. Solsona
- FECEC (FEDERACIÓ CATALANA D’ENTITATS CONTRA EL CÁNCER
- FUNDACIÓ KÁLIDA. Barcelona
- FUNDACIÓ ROSES CONTRA EL CÀNCER. Roses
- LLIGA CONTRA EL CÀNCER COMARQUES DE TARRAGONA I TERRES DE L’EBRE. Tarragona
- MielomaCAT
- ONCOLLIGA BARCELONA. Barcelona
- ONCOLLIGA GIRONA. Girona
- ONCOLLIGA COMARQUES DE LLEIDA. Lleida
- ONCOVALLÈS. Vallès Oriental
- OSONA CONTRA EL CÀNCER. Osona
- SUPORT I COMPANYIA. Barcelona
- VILASSAR DE DALT CONTRA EL CÀNCER. Vilassar de Dalt
VALENCIAN COMMUNITY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASLEUVAL (ASOCIACIÓN DE PACIENTES DE LEUCEMIA, LINFOMA, MIELOMA Y OTRAS ENFERMEDADES DE LA SANGRE DE VALENCIA)
EXTREMADURA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- AFAL (AYUDA A FAMILIAS AFECTADAS DE LEUCEMIAS, LINFOMAS; MIELOMAS Y APLASIAS)
- AOEX (ASOCIACIÓN ONCOLÓGICA EXTREMEÑA)
GALICIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASOTRAME (ASOCIACIÓN GALLEGA DE AFECTADOS POR TRASPLANTES MEDULARES)
BALEARIC ISLANDS
- ADAA (ASSOCIACIÓ D’AJUDA A L’ACOMPANYAMENT DEL MALALT DE LES ILLES BALEARS)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
CANARY ISLANDS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- AFOL (ASOCIACIÓN DE FAMILIAS ONCOHEMATOLÓGICAS DE LANZAROTE)
- FUNDACIÓN ALEJANDRO DA SILVA
LA RIOJA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
MADRID
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- AEAL (ASOCIACIÓN ESPAÑOLA DE LEUCEMIA Y LINFOMA)
- CRIS CONTRA EL CÁNCER
- FUNDACIÓN LEUCEMIA Y LINFOMA
MURCIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
NAVARRA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
BASQUE COUNTRY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- PAUSOZ-PAUSO. Bilbao
AUTONOMOUS CITIES OF CEUTA AND MELILLA
- AECC CEUTA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
- AECC MELILLA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
Support and assistance
We also invite you to follow us through our main social media (Facebook, Twitter and Instagram) where we often share testimonies of overcoming this disease.
If you live in Spain, you can also contact us by sending an e-mail to imparables@fcarreras.es so that we can help you get in touch with other people who have overcome this disease.
* In accordance with Law 34/2002 on Information Society Services and Electronic Commerce (LSSICE), the Josep Carreras Leukemia Foundation informs that all medical information available on www.fcarreras.org has been reviewed and accredited by Dr. Enric Carreras Pons, Member No. 9438, Barcelona, Doctor in Medicine and Surgery, Specialist in Internal Medicine, Specialist in Hematology and Hemotherapy and Senior Consultant of the Foundation; and by Dr. Rocío Parody Porras, Member No. 35205, Barcelona, Doctor in Medicine and Surgery, Specialist in Hematology and Hemotherapy and attached to the Medical Directorate of the Registry of Bone Marrow Donors (REDMO) of the Foundation).
Become a member of the cure for leukaemia!


