Cutaneous T-cell lymphomas
The information provided on www.fcarreras.org is intended to support, not replace, the relationship that exists between patients/visitors to this website and their physician.
Information reviewed by Dr. Rocío Parody Porras, Doctor specialising in Haematology. Member of the Management of REDMO (Bone Marrow Donor Registry) and of the Foundation’s medical team. Barcelona Medical Association (Co. 35205)
What are cutaneous T-cell lymphomas?
 There are several types of cutaneous T-cell lymphoma. The most common type is Mycosis fungoides (MF) and the most severe type is Sézary syndrome (SSZ). In this section, we will focus on these two subtypes, which account for about 75-80% of all cutaneous T-cell lymphomas. Mycosis fungoides is a rare type of lymphoma diagnosed in about 200 people each year in Spain. Despite being uncommon, it is the most common cutaneous lymphoma and accounts for approximately 50% of new cutaneous lymphoma diagnoses.
There are several types of cutaneous T-cell lymphoma. The most common type is Mycosis fungoides (MF) and the most severe type is Sézary syndrome (SSZ). In this section, we will focus on these two subtypes, which account for about 75-80% of all cutaneous T-cell lymphomas. Mycosis fungoides is a rare type of lymphoma diagnosed in about 200 people each year in Spain. Despite being uncommon, it is the most common cutaneous lymphoma and accounts for approximately 50% of new cutaneous lymphoma diagnoses.
Mycosis fungoides (MF) affects both sexes equally. Until a few years ago it was said to affect mainly in later life, from the age of 50-60 years. With new diagnostic methods, it is increasingly diagnosed in younger patients with early lesions.
Cutaneous T-cell lymphomas are a type of non-Hodgkin’s T-cell lymphoma with a chronic course in which T-lymphocytes become abnormal and start attacking the skin. These lymphomas are called “cutaneous primary” because their first manifestation is in the skin.
The Sézary Syndrome is an aggressive type of cutaneous T-cell lymphoma that also manifests in the blood. It can originate from a previous mycosis fungoides.
The Sézary Syndrome (SSZ) mainly affects people between 60 and 70 years of age. It affects more men than women in a ratio of 2:1. The International Society for Cutaneous Lymphoma (SILC) and the European Organisation for Research and Treatment of Cancer (EOCTC) define the Sézary syndrome as the leukaemic phase of cutaneous T-cell lymphoma. This variant of cutaneous T-cell lymphoma occurs with an annual incidence of 1/10,000,000 people. Therefore, in Spain we could say that around 50 people are diagnosed with Sézary Syndrome each year.
As with most lymphomas, the causes are unknown. In terms of clinical manifestations and diagnosis, it has its own distinctive features compared to other lymphomas, as detailed below:
What are the symptoms of cutaneous T-cell lymphomas?
In MF, the first symptom is usually redness of the skin, called erythema, sometimes in the form of persistent, scaly, erythematous macules. It has an indolent course (i.e. it is not aggressive in its development) but is progressive over time. The initial manifestations can be very non-specific and persist for months and years. In fact, it can be mistaken for eczema that does not respond to treatment, with contact dermatitis, allergies to certain substances, psoriasis, etc. A biopsy of the lesions is necessary to confirm it. Very rarely tumour formation is already present at the onset of the disease.
On the other hand, SSZ is characterised by what is known as the triad:
- Erythroderma: is a generalised exfoliative skin inflammation, involving 90% or more of the patient’s skin. Erythroderma is potentially severe, and patients may require hospitalisation to control and restore fluid and electrolyte balance, circulatory status and body temperature.
- Lymphadenopathy: swollen lymph nodes.
- Circulating atypical lymphocytes (Sézary cells): these are atypical T-lymphocytes that will be seen in the peripheral blood or circulating blood.
How are cutaneous T-cell lymphomas diagnosed?
The phases of mycosis fungoides can be categorised as:
- Premycotic phase: a reddish, scaly rash appears on parts of the body not exposed to the sun, especially the torso. This rash produces no symptoms and may last for months or years. During this phase, it is very difficult for the rash to be diagnosed as Mycosis Fungoides.
- Patchy phase: a fine, reddish rash that looks like eczema is present.
- Plaque phase: small raised bumps (papules) or hard lesions appear on the skin, which are sometimes reddened.
- Tumour phase: tumours form on the skin. Sometimes ulcers develop in these tumours and the skin becomes infected.
In the case of Sézary Syndrome (SSZ), laboratory tests and histopathology, which is essential for detecting Sézary cells, are used to confirm the diagnosis. Immunohistochemical and immunogenetic techniques are of vital importance for diagnosis, as well as absolute Sézary cell count (≥1000/μl).
Sézary syndrome and mycosis fungoides share a staging system based on the determination of the degree of cutaneous (T), lymph node (N), visceral (M) and peripheral blood (B) involvement.
Since its review by the EORTC/ISCL in 2007, patients with Sézary Syndrome correspond to the T4 (cutaneous involvement of more than 80%) and B2 (≥1,000 Sézary cells) forms.

What is the treatment for cutaneous T-cell lymphomas?
In mycosis fungoides, apart from the non-specific symptoms of the early stages, treatment can be directed only at the skin. There is no need for very aggressive systemic or chemotherapeutic treatments as it has been shown that disease survival is the same, or even worse, if patients are treated aggressively from the outset than if more conservative treatments are used.
In the very early stages, patients may not even require phototherapy treatment, but can use potent corticosteroid creams (such as clobetasol) and monitoring. The therapeutic approach is to avoid side effects. It is a ‘wait and see’ treatment.
If the disease progresses and the patient has advanced skin lesions, tumours, lesions appear, lymph nodes, then a two-fold treatment is necessary: on the one hand directed at the skin and, on the other hand, extra cutaneous.
In international guidelines, phototherapy with UVB or PUVA are recommended as first line therapy in patients with early stage Mycosis Fungoides and as part of combined treatments in more advanced stages. Depending on the patient, the specialist decides whether to treat with UVB or UVA depending on the patient and the type of lesions. The specialist will also assess other treatments such as oral retinoids or topical treatments such as bexarotene, which is used both in the early stages as a complementary treatment and in the more advanced stages. In patients who have very extensive lesions but only localised to the skin, total body irradiation with electrons can also be applied. It would be like a further step of phototherapy without being conventional radiotherapy.
Quality of life is one of the main objectives. Maximising periods of disease remission or stabilisation is a priority, as well as minimising treatment effects and toxicity.
Treatment of SSZ is always mixed: skin and systemic, and the overall results are poor and never curative. Standard treatment consists of phototherapy (extracorporeal photopheresis, which is a procedure that removes circulating tumour cells) and, chemotherapy (chlorambucil, methotrexate and pentostatin):
- Also, topical corticosteroids are used to alleviate skin symptomatology (inflammation and itching).
- The retinoids, such as bexarotene, are drugs that are related to vitamin A and delay the multiplication of certain types of cancer cells. In Spain, it is approved for oral use in patients with advanced forms refractory to at least one previous line of treatment. It is a slow-acting drug with a median response time of approximately 20 weeks, so it is recommended to maintain treatment for at least 6 months.
- Extracorporeal photochemotherapy or photopheresis is approved by the FDA in the United States for the treatment of extensive MF and SS. It is frequently used in Spain, alone or in combination. The technique consists of oral administration of 8-methoxypsoralen (8-MOP), followed by leukocyte apheresis with extracorporeal UVA irradiation and reinfusion of the cells back into the patient (thereby stimulating the immune system and eliminating tumour T-lymphocytes). It is a technique that requires good peripheral access or central venous access. It can be maintained for months or years.
- Monoclonal antibodies, i.e. directed against specific molecules expressed by the lymphoma, which are basically:
- Brentuximab vedotin (BV) has conditional approval by the EMA for the treatment of adult patients with CD30+ cutaneous T-cell lymphoma (CTCL) after at least one systemic treatment.
- Mogalizumab, is the first drug to receive a specific indication by the EMA for the treatment of SSZ and MF after at least one prior systemic treatment. This drug targets a specific molecule called CCR4. This drug can only be given in experienced centres. Administration is weekly, on days 1, 8, 15 and 22 of the first 28-day cycle, followed by infusions every two weeks on days 1 and 15 of each subsequent 28-day cycle, until disease progression or unacceptable toxicity. Premedication (antipyretic and antihistamine) is recommended to avoid infusion reactions.
- Alemtuzumab, targeting CD52, which has no indication but could be used on special request.
- Other drugs such as Romidepsin or Vorinostat, which are not currently approved in Europe and would have to be accessed on a compassionate use basis.
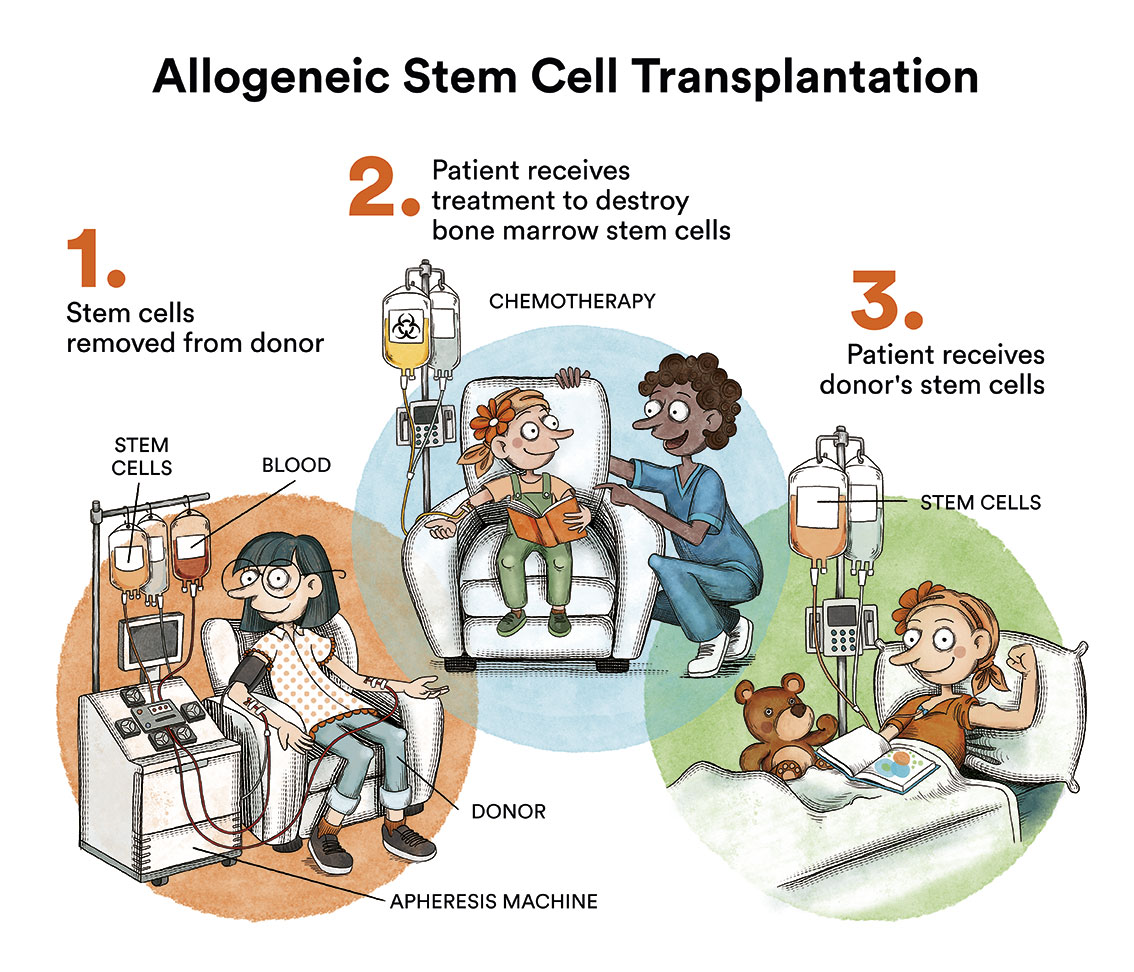
An allogeneic haematopoietic stem cell transplantation may be indicated in young patients with advanced disease (MF and SSZ), although the results are limited due to the low remission rate and high mortality of the procedure.
What are the chances of patients with cutaneous T-cell lymphomas being cured?
Mycosis fungoides is not a curable disease today. Most patients do not progress or remain at an early stage with plaque lesions. In about 10% of cases progression to advanced cutaneous (tumour) and extra cutaneous (lymph nodes, viscera, blood) disease occurs. Only a minority of patients with Mycosis Fungoides die from their disease. They are long-term patients who can live with the disease for more than 20 years, with a very good prognosis.
The prognosis of the Sézary Syndrome (SSZ) is poor, with the median survival of patients being approximately 5 years, depending on the initial presentation and its evolution.
Links of interest concerning medical issues relating to cutaneous T-cell lymphomas
Cutaneous T-Cell Lymphoma. Lymphoma research Foundation
Cutaneous T-cell lymphoma (CTCL). Macmillan Cancer Support
Mycosis Fungoides (Including Sézary Syndrome) Treatment. National Cancer Institute
Sézary Syndrome. Cleveland Clinic
Links of interest on other topics related to non-Hodgkin’s lymphoma:
TESTIMONIAL MATERIALS
You can order the booklets in paper format for free delivery in Spain by e-mail: imparables@fcarreras.es
BONE MARROW TRANSPLANT
- Bone Marrow Transplant Guide. Josep Carreras Foundation (content in Spanish)
- What is HLA and how does it work? Josep Carreras Foundation (content in Spanish)
- Graft-versus-Host Disease. Josep Carreras Foundation (content in Spanish)
- History of Bone Marrow Transplantation. Josep Carreras Foundation (content in Spanish)
- How is the search for an anonymous donor conducted? Josep Carreras Foundation (content in Spanish)
FOOD
- How to maintain a healthy diet during treatment? Josep Carreras Foundation (content in Spanish)
- Nutrition guide. Leukemia & Lymphoma Society
OTHER
- Ideas on what to take with me to the isolation chamber. Josep Carreras Leukaemia Foundation (content in Spanish)
- Travel tips for people with cancer. Josep Carreras Leukaemia Foundation (content in Spanish)
- Physiotherapy manual for haematological and transplant patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Prevention and treatment of oral mucositis. Josep Carreras Leukaemia Foundation (content in Spanish)
- Oral hygiene in oncohaematological patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Fertility manual: Suffering from blood cancer and becoming a parent. Josep Carreras Leukaemia Foundation (content in Spanish)
- Skin care in the oncohaematological patient. Josep Carreras Leukaemia Foundation (content in Spanish)
- Aesthetic Oncology Manual. Josep Carreras Leukaemia Foundation (content in Spanish)
- Leukaemia and sexuality. Josep Carreras Leukaemia Foundation (content in Spanish)
- 7 ways to wear a scarf. Josep Carreras Leukaemia Foundation (content in Spanish)
Links of interest: local/provincial or state entities that can provide you with resources and services specialised in leukaemia, lymphoma or cancer patients:
In Spain there is a large network of associations for haematological cancer patients which, in many cases, can provide information, advice and even carry out certain procedures. These are the contacts of some of them by Autonomous Community:
All these organisations are external to the Josep Carreras Foundation.
STATE
- AMILO (Asociación Española de Amiloidosis)
- ACLIF (Asociación para la cura del linfoma folicular)
- AEAL (ASOCIACIÓN ESPAÑOLA DE AFECTADOS POR LINFOMA, MIELOMA y LEUCEMIA)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch or call 900 100 036 (24h).
- AELCLES (Agrupación Española contra la Leucemia y Enfermedades de la Sangre)
- CEMMP (Comunidad Española de Pacientes de Mieloma Múltiple)
- JOSEP CARRERAS LEUKAEMIA FOUNDATION
- FUNDACIÓN SANDRA IBARRA
- GEPAC (GRUPO ESPAÑOL DE PACIENTES CON CÁNCER)
- MPN España (Asociación de Afectados Por Neoplasias Mieloproliferativas Crónicas)
ANDALUCÍA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ALUSVI (ASOCIACIÓN LUCHA Y SONRÍE POR LA VIDA). Sevilla
- APOLEU (ASOCIACIÓN DE APOYO A PACIENTES Y FAMILIARES DE LEUCEMIA). Cádiz
ARAGÓN
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASPHER (ASOCIACIÓN DE PACIENTES DE ENFERMEDADES HEMATOLÓGICAS RARAS DE ARAGÓN)
- DONA MÉDULA ARAGÓN
ASTURIAS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASTHEHA (ASOCIACIÓN DE TRASPLANTADOS HEMATOPOYÉTICOS Y ENFERMOS HEMATOLÓGICOS DE ASTURIAS)
CANTABRIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LA MANCHA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LEÓN
- ABACES (ASOCIACIÓN BERCIANA DE AYUDA CONTRA LAS ENFERMEDADES DE LA SANGRE)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ALCLES (ASOCIACIÓN LEONESA CON LAS ENFERMEDADES DE LA SANGRE). León.
- ASCOL (ASOCIACIÓN CONTRA LA LEUCEMIA Y ENFERMEDADES DE LA SANGRE). Salamanca.
CATALUÑA
- ASSOCIACIÓ FÈNIX. Solsona
- FECEC (FEDERACIÓ CATALANA D’ENTITATS CONTRA EL CÁNCER
- FUNDACIÓ KÁLIDA. Barcelona
- FUNDACIÓ ROSES CONTRA EL CÀNCER. Roses
- LLIGA CONTRA EL CÀNCER COMARQUES DE TARRAGONA I TERRES DE L’EBRE. Tarragona
- MielomaCAT
- ONCOLLIGA BARCELONA. Barcelona
- ONCOLLIGA GIRONA. Girona
- ONCOLLIGA COMARQUES DE LLEIDA. Lleida
- ONCOVALLÈS. Vallès Oriental
- OSONA CONTRA EL CÀNCER. Osona
- SUPORT I COMPANYIA. Barcelona
- VILASSAR DE DALT CONTRA EL CÀNCER. Vilassar de Dalt
VALENCIAN COMMUNITY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASLEUVAL (ASOCIACIÓN DE PACIENTES DE LEUCEMIA, LINFOMA, MIELOMA Y OTRAS ENFERMEDADES DE LA SANGRE DE VALENCIA)
EXTREMADURA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AFAL (AYUDA A FAMILIAS AFECTADAS DE LEUCEMIAS, LINFOMAS; MIELOMAS Y APLASIAS)
- AOEX (ASOCIACIÓN ONCOLÓGICA EXTREMEÑA)
GALICIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASOTRAME (ASOCIACIÓN GALLEGA DE AFECTADOS POR TRASPLANTES MEDULARES)
BALEARIC ISLANDS
- ADAA (ASSOCIACIÓ D’AJUDA A L’ACOMPANYAMENT DEL MALALT DE LES ILLES BALEARS)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CANARY ISLANDS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AFOL (ASOCIACIÓN DE FAMILIAS ONCOHEMATOLÓGICAS DE LANZAROTE)
- FUNDACIÓN ALEJANDRO DA SILVA
LA RIOJA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
MADRID
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AEAL (ASOCIACIÓN ESPAÑOLA DE LEUCEMIA Y LINFOMA)
- CRIS CONTRA EL CÁNCER
- FUNDACIÓN LEUCEMIA Y LINFOMA
MURCIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
NAVARRA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
BASQUE COUNTRY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- PAUSOZ-PAUSO. Bilbao
AUTONOMOUS CITIES OF CEUTA AND MELILLA
- AECC CEUTA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
- AECC MELILLA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
Support and assistance
We also invite you to follow us through our main social media (Facebook, Twitter and Instagram) where we often share testimonies of overcoming this disease.
If you live in Spain, you can also contact us by sending an e-mail to imparables@fcarreras.es so that we can help you get in touch with other people who have overcome this disease.
* In accordance with Law 34/2002 on Information Society Services and Electronic Commerce (LSSICE), the Josep Carreras Leukemia Foundation informs that all medical information available on www.fcarreras.org has been reviewed and accredited by Dr. Enric Carreras Pons, Member No. 9438, Barcelona, Doctor in Medicine and Surgery, Specialist in Internal Medicine, Specialist in Hematology and Hemotherapy and Senior Consultant of the Foundation; and by Dr. Rocío Parody Porras, Member No. 35205, Barcelona, Doctor in Medicine and Surgery, Specialist in Hematology and Hemotherapy and attached to the Medical Directorate of the Registry of Bone Marrow Donors (REDMO) of the Foundation).
Become a member of the cure for leukaemia!


