Peripheral T-cell lymphomas
The information provided on www.fcarreras.org is intended to support, not replace, the relationship that exists between patients/visitors to this website and their physician.

Alejandro
Angioimmunoblastic T lymphoma.
“I have been unstoppable against lymphoma since 2007. I was diagnosed with non-Hodgkin lymphoma and underwent an autotransplant in 2009. I was in complete remission for two years until I relapsed again. That’s when the Josep Carreras Foundation came into my life. I needed an anonymous bone marrow donor who was 100% compatible with me because none of my siblings were. If there is something that has helped me all this time and continues to help me, it is my sense of humor. The people, their smiles, being able to enjoy and have a good time.”
Information reviewed by Dr. Rocío Parody Porras, Doctor specialising in Haematology. Member of the Management of REDMO (Bone Marrow Donor Registry) and of the Foundation’s medical team. Barcelona Medical Association (Co. 35205)
What are peripheral T-cell lymphomas?
Peripheral T-cell lymphomas are a heterogeneous group of non-Hodgkin’s lymphomas of complex diagnosis and relatively low incidence (10-15% of non-Hodgkin’s lymphomas in the Western world). They are rare entities and usually have an aggressive and rapid course. Overall, they account for about 10% of all non-Hodgkin’s lymphomas and usually affect people over the age of 60, although they can sometimes be identified in children and young adults.
To understand what peripheral T-cell lymphomas are, it is important to understand how and where a T lymphocyte matures.
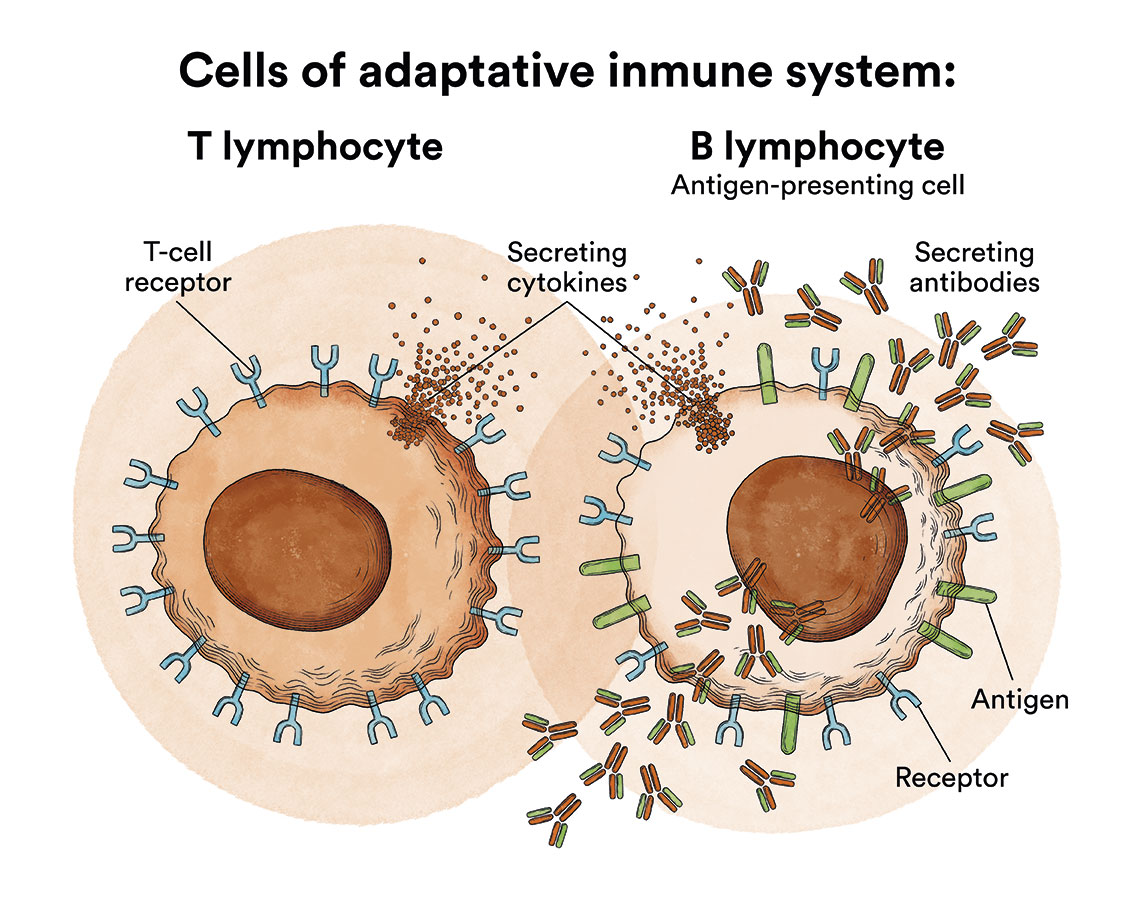
Let us recall that T lymphocytes are a fundamental part of the human body’s immune system and are formed, like B lymphocytes, in the bone marrow. But then the T lymphocytes go to thymus to mature.
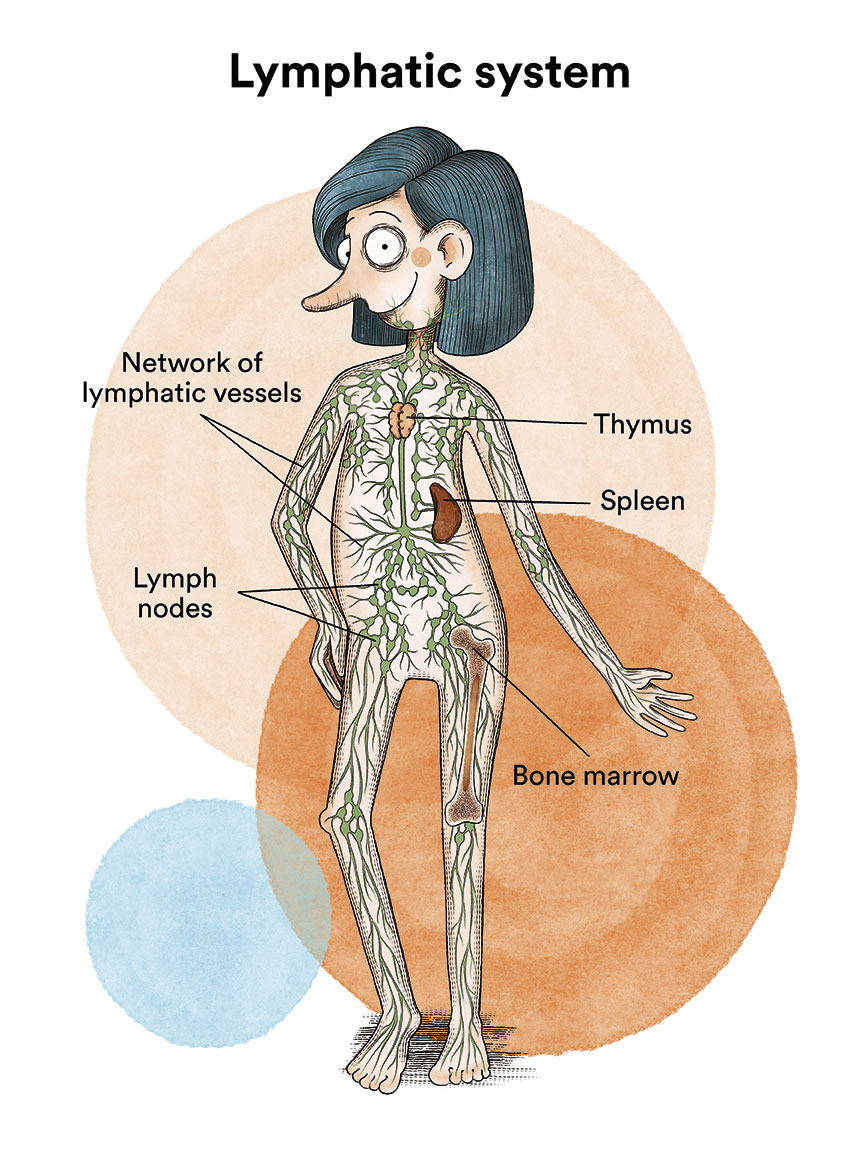
These immature T lymphocytes that go to the thymus and mature there are called thymocytes. These lymphocytes will then move into the blood and lymphatic system (moving to the periphery) until they are activated when they come into contact with a specific antigen. They are called activated T lymphocytes and will be responsible for cell-mediated immunity, destroying foreign cells or activating other cells to enhance immunity.
Peripheral T-cell lymphomas arise in these mature T lymphocytes that have migrated from the thymus to the periphery and are responsible for the cell-mediated immune response.
Although there are more than 20 subtypes of peripheral T-cell lymphomas, the World Health Organization classification divides peripheral T-cell lymphomas into two major groups:
- Peripheral T-cell lymphomas with nodal predominance (involved lymph nodes). In this group, the most common peripheral T-cell lymphomas are anaplastic T-cell lymphoma, the angioimmunoblastic T-cell lymphoma and the unspecified peripheral T-cell lymphomas.
- Anaplastic T-cell lymphoma: this type of lymphoma, in general, has the best prognosis of these nodal peripheral T-cell lymphomas. A typical diagnostic feature of these lymphomas is the expression of the CD30 antigen on the cell surface of the lymphoma cell. See previous section Anaplastic large cell lymphoma.
- Angioimmunoblastic T-cell lymphoma: constitutes about 20% of peripheral T-cell lymphomas.
- Peripheral T-cell lymphomas not otherwise specified: is a heterogeneous entity that includes T-cell lymphomas that could not be classified. It is therefore a “catch-all” that represents about 55% of these peripheral T-cell lymphomas and is the most frequent T-cell lymphoma in Western countries.
- Peripheral T-cell lymphomas with extra-nodal predominance (other extraganglionic, “non-lymphoid” organs affected: skin, liver, spleen, intestine…). The most numerous in this group are cutaneous lymphomas. We will explain cutaneous T-cell lymphomas separately in a corresponding section.
Among the other non-cutaneous locations, and although they are infrequent entities, the following predominate:
- Enteropathic T-cell lymphoma: predominantly affects adults from 50-60 years of age with a history of coeliac disease. Its clinical course is localised in the small intestine and is aggressive.
- Panniculitic T-lymphoma: forms in subcutaneous nodules and mainly affects older women.
- Hepatosplenic T-lymphoma: preferentially affects young males and presents with an enlarged spleen and liver (hepatosplenomegaly).
The causes of T-lymphomas are unknown. Regarding symptoms, it depends on each type of lymphoma specified above, as the involvement can be nodal or extranodal (as occurs in enteropathic, panniculitic, hepatosplenic)
Regarding diagnosis and extension studies, is common to all other non-Hodgkin’s lymphomas (NHL), with biopsy of the lymph node and/or affected tissue being essential, with immunophenotyping, cytogenetic and molecular studies (the latter two being particularly important for anaplastic lymphoma).
On the other hand, each person is categorised into a prognostic risk group according to a score called IPI (International Prognostic Index) which considers the following variables: age (over or under 60 years), localised stage (1-2) vs. advanced (3-4), extranodal involvement (2 or more sites), general condition (measured by an index called ECOG) as well as elevated serum lactate dehydrogenase level.

Esther
Anaplastic T cell lymphoma.
“On December 21, 2018, when I was 23 years old, I was diagnosed with non-Hodgkin lymphoma. We thought it would be quick, but everything got complicated… ¿The summary? 3 relapses, 4 lines of treatment, 2 admissions to the ICU, other eternal admissions, 2 transplants and a pandemic in between, as if that were not enough. Luckily, thanks to my brother’s bone marrow donation, I am cured. After all the treatment, today I have returned to experiencing first times, I have returned to the gym, I have returned to work, I have returned to studying, I have returned to hugging, kissing and feeling. Probably only few patients will experience everything that happened to me but, for them, I would like that my testimony gives them hope.”
What is the treatment for peripheral T-cell lymphomas?
In this section we will consider peripheral T-cell lymphomas in general and add characteristics specific to each one below.
In general, most peripheral T-cell lymphomas are treated with conventional combination chemotherapy: chemotherapy with CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone) or CHOEP (clophosphamide, doxorubicin, vincristine, etoposide and prednisone) regimen, administered every 2-3 weeks for a total of 6 cycles.
 In most cases of peripheral T-cell lymphomas of nodal development (the disease is located within the lymph nodes), combinations of chemotherapy (cyclophosphamide, doxorubicin and prednisone) together with Brentuximab vedotin (Adcetris®) will be used. Brentuximab vedotin is a CD30-targeted monoclonal antibody and therefore indicated for CD30-expressing lymphomas such as angioimmunoblastic T-cell lymphoma and peripheral T-cell lymphoma not otherwise specified.
In most cases of peripheral T-cell lymphomas of nodal development (the disease is located within the lymph nodes), combinations of chemotherapy (cyclophosphamide, doxorubicin and prednisone) together with Brentuximab vedotin (Adcetris®) will be used. Brentuximab vedotin is a CD30-targeted monoclonal antibody and therefore indicated for CD30-expressing lymphomas such as angioimmunoblastic T-cell lymphoma and peripheral T-cell lymphoma not otherwise specified.
In cases of refractoriness or relapse, standard protocols have not yet been established but different drugs are being tested on a clinical trial basis. Some commonly used treatment regimens for relapsed or refractory disease are:
- ICE: ifosfamide, carboplatin, etoposide
- DHAP: dexamethasone, cisplatin, cytarabine
- ESHAP: etoposide, methylprednisolone, cytarabine, cisplatin
- GemOx: gemcitabine, oxaliplatin
- GDP: gemcitabine, dexamethasone, cisplatin
- GVD: gemcitabine, vinorelbine, liposomal doxorubicin
Some patients with peripheral T-cell lymphoma may benefit from undergoing, after initial chemotherapy, an autologous stem cell transplant, such as patients considered high risk, up to 70 years of age, and with chemosensitive disease (i.e. who have responded to prior chemotherapy treatment). Allogeneic (donor) transplantation is reserved for young patients (<70 years) after relapse in aggressive subtypes of T-cell lymphomas.
Let us now review the most common types of peripheral T-cell lymphomas and their specific treatment strategy.
- Nodal predominant peripheral T-cell lymphomas (lymph nodes involved):
- Anaplastic T-cell lymphoma
- The peripheral T-cell lymphoma not otherwise specified: its course is aggressive and requires immediate treatment. All patients should be assessed for CD30 expression on affected cells, in which case brentuximab vedotin in combination with chemotherapy CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) would be indicated.
- The angioimmunoblastic T-cell lymphoma: Brentuximab vedotin is approved for the treatment of CD30-expressing angioimmunoblastic T-cell lymphoma in previously untreated cases in combination with cyclophosphamide, doxorubicin and prednisone. Some patients are treated with standard chemotherapy followed by autologous stem cell transplantation. The use of new combinations of chemotherapy drugs, either with or without stem cell transplantation, is being evaluated in clinical trials.
- Peripheral T-lymphomas of extra-nodal predominance:
- Enteropathic T-lymphoma (or Enteropathy-associated T-cell lymphoma or intestinal T-cell lymphoma): includes regimens of chemotherapy as CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) or more intensive regimens. Treatment may include bowel surgery and an autologous stem cell transplant . A gluten-free diet is recommended in these patients.
- Panniculitic T-cell lymphoma: less intensive treatment (low-dose methotrexate or immunosuppressive therapy) is usually used.
- Hepatosplenic T-cell lymphoma: includes chemotherapy regimens such as CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) and, in most cases, autologous bone marrow transplantation. If relapse occurs or in patients in whom remission is achieved, allogeneic stem cell transplantation may be included.
What are the chances of patients with peripheral T-cell lymphomas being cured?
Compared to B-type lymphomas, T-type lymphomas generally have a poorer prognosis. Due to their low prevalence and complicated prognosis (with the exception of anaplastic ALK+ or cutaneous T-lymphomas), peripheral T-lymphomas currently represent a research challenge. Overall, conventional therapy offers 20-30% prolonged survival. Despite this, numerous clinical trials are currently underway and should be considered.
As mentioned above, some types of peripheral T-cell lymphoma are more frequently associated with better prognoses than others. These include: anaplastic large cell lymphoma (ALCL) with ALK (anaplastic lymphoma kinase) abnormality and anaplastic large cell lymphoma without ALK abnormality, when treated with brentuximab vedotin and chemotherapy; as well as extranodal NK-cell or T-cell lymphoma in cases of localised disease, for which localised radiotherapy and anthracycline-based chemotherapy is usually recommended.
Links of interest concerning medical issues relating to peripheral T-cell lymphomas
Peripheral T-Cell Lymphoma. Lymphoma research Foundation
Peripheral T-Cell Lymphoma (PTCL). Cleveland Clinic
Peripheral T-Cell Lymphoma. Leukemia & Lymphoma Foundation
Peripheral T-cell lymphoma, not otherwise specified (PTCL-NOS). Macmillan Cancer Support
Links of interest on other topics related to non-Hodgkin’s lymphoma:
TESTIMONIAL MATERIALS
You can order the booklets in paper format for free delivery in Spain by e-mail: imparables@fcarreras.es
BONE MARROW TRANSPLANT
- Bone Marrow Transplant Guide. Josep Carreras Foundation (content in Spanish)
- What is HLA and how does it work? Josep Carreras Foundation (content in Spanish)
- Graft-versus-Host Disease. Josep Carreras Foundation (content in Spanish)
- History of Bone Marrow Transplantation. Josep Carreras Foundation (content in Spanish)
- How is the search for an anonymous donor conducted? Josep Carreras Foundation (content in Spanish)
FOOD
- How to maintain a healthy diet during treatment? Josep Carreras Foundation (content in Spanish)
- Nutrition guide. Leukemia & Lymphoma Society
OTHER
- Ideas on what to take with me to the isolation chamber. Josep Carreras Leukaemia Foundation (content in Spanish)
- Travel tips for people with cancer. Josep Carreras Leukaemia Foundation (content in Spanish)
- Physiotherapy manual for haematological and transplant patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Prevention and treatment of oral mucositis. Josep Carreras Leukaemia Foundation (content in Spanish)
- Oral hygiene in oncohaematological patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Fertility manual: Suffering from blood cancer and becoming a parent. Josep Carreras Leukaemia Foundation (content in Spanish)
- Skin care in the oncohaematological patient. Josep Carreras Leukaemia Foundation (content in Spanish)
- Aesthetic Oncology Manual. Josep Carreras Leukaemia Foundation (content in Spanish)
- Leukaemia and sexuality. Josep Carreras Leukaemia Foundation (content in Spanish)
- 7 ways to wear a scarf. Josep Carreras Leukaemia Foundation (content in Spanish)
Links of interest: local/provincial or state entities that can provide you with resources and services specialised in leukaemia, lymphoma or cancer patients:
In Spain there is a large network of associations for haematological cancer patients which, in many cases, can provide information, advice and even carry out certain procedures. These are the contacts of some of them by Autonomous Community:
All these organisations are external to the Josep Carreras Foundation.
STATE
- AMILO (Asociación Española de Amiloidosis)
- ACLIF (Asociación para la cura del linfoma folicular)
- AEAL (ASOCIACIÓN ESPAÑOLA DE AFECTADOS POR LINFOMA, MIELOMA y LEUCEMIA)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch or call 900 100 036 (24h).
- AELCLES (Agrupación Española contra la Leucemia y Enfermedades de la Sangre)
- CEMMP (Comunidad Española de Pacientes de Mieloma Múltiple)
- JOSEP CARRERAS LEUKAEMIA FOUNDATION
- FUNDACIÓN SANDRA IBARRA
- GEPAC (GRUPO ESPAÑOL DE PACIENTES CON CÁNCER)
- MPN España (Asociación de Afectados Por Neoplasias Mieloproliferativas Crónicas)
ANDALUCÍA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ALUSVI (ASOCIACIÓN LUCHA Y SONRÍE POR LA VIDA). Sevilla
- APOLEU (ASOCIACIÓN DE APOYO A PACIENTES Y FAMILIARES DE LEUCEMIA). Cádiz
ARAGÓN
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASPHER (ASOCIACIÓN DE PACIENTES DE ENFERMEDADES HEMATOLÓGICAS RARAS DE ARAGÓN)
- DONA MÉDULA ARAGÓN
ASTURIAS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASTHEHA (ASOCIACIÓN DE TRASPLANTADOS HEMATOPOYÉTICOS Y ENFERMOS HEMATOLÓGICOS DE ASTURIAS)
CANTABRIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LA MANCHA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LEÓN
- ABACES (ASOCIACIÓN BERCIANA DE AYUDA CONTRA LAS ENFERMEDADES DE LA SANGRE)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ALCLES (ASOCIACIÓN LEONESA CON LAS ENFERMEDADES DE LA SANGRE). León.
- ASCOL (ASOCIACIÓN CONTRA LA LEUCEMIA Y ENFERMEDADES DE LA SANGRE). Salamanca.
CATALUÑA
- ASSOCIACIÓ FÈNIX. Solsona
- FECEC (FEDERACIÓ CATALANA D’ENTITATS CONTRA EL CÁNCER
- FUNDACIÓ KÁLIDA. Barcelona
- FUNDACIÓ ROSES CONTRA EL CÀNCER. Roses
- LLIGA CONTRA EL CÀNCER COMARQUES DE TARRAGONA I TERRES DE L’EBRE. Tarragona
- MielomaCAT
- ONCOLLIGA BARCELONA. Barcelona
- ONCOLLIGA GIRONA. Girona
- ONCOLLIGA COMARQUES DE LLEIDA. Lleida
- ONCOVALLÈS. Vallès Oriental
- OSONA CONTRA EL CÀNCER. Osona
- SUPORT I COMPANYIA. Barcelona
- VILASSAR DE DALT CONTRA EL CÀNCER. Vilassar de Dalt
VALENCIAN COMMUNITY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASLEUVAL (ASOCIACIÓN DE PACIENTES DE LEUCEMIA, LINFOMA, MIELOMA Y OTRAS ENFERMEDADES DE LA SANGRE DE VALENCIA)
EXTREMADURA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AFAL (AYUDA A FAMILIAS AFECTADAS DE LEUCEMIAS, LINFOMAS; MIELOMAS Y APLASIAS)
- AOEX (ASOCIACIÓN ONCOLÓGICA EXTREMEÑA)
GALICIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- ASOTRAME (ASOCIACIÓN GALLEGA DE AFECTADOS POR TRASPLANTES MEDULARES)
BALEARIC ISLANDS
- ADAA (ASSOCIACIÓ D’AJUDA A L’ACOMPANYAMENT DEL MALALT DE LES ILLES BALEARS)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
CANARY ISLANDS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AFOL (ASOCIACIÓN DE FAMILIAS ONCOHEMATOLÓGICAS DE LANZAROTE)
- FUNDACIÓN ALEJANDRO DA SILVA
LA RIOJA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
MADRID
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- AEAL (ASOCIACIÓN ESPAÑOLA DE LEUCEMIA Y LINFOMA)
- CRIS CONTRA EL CÁNCER
- FUNDACIÓN LEUCEMIA Y LINFOMA
MURCIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
NAVARRA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
BASQUE COUNTRY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present in the different provinces and in many municipalities. Contact the nearest branch.
- PAUSOZ-PAUSO. Bilbao
AUTONOMOUS CITIES OF CEUTA AND MELILLA
- AECC CEUTA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
- AECC MELILLA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
Support and assistance
We also invite you to follow us through our main social media (Facebook, Twitter and Instagram) where we often share testimonies of overcoming this disease.
If you live in Spain, you can also contact us by sending an e-mail to imparables@fcarreras.es so that we can help you get in touch with other people who have overcome this disease.
* In accordance with Law 34/2002 on Information Society Services and Electronic Commerce (LSSICE), the Josep Carreras Leukemia Foundation informs that all medical information available on www.fcarreras.org has been reviewed and accredited by Dr. Enric Carreras Pons, Member No. 9438, Barcelona, Doctor in Medicine and Surgery, Specialist in Internal Medicine, Specialist in Hematology and Hemotherapy and Senior Consultant of the Foundation; and by Dr. Rocío Parody Porras, Member No. 35205, Barcelona, Doctor in Medicine and Surgery, Specialist in Hematology and Hemotherapy and attached to the Medical Directorate of the Registry of Bone Marrow Donors (REDMO) of the Foundation).
Become a member of the cure for leukaemia!


