Polycythaemia vera
The information provided on www.fcarreras.org is intended to support, not replace, the relationship that exists between patients/visitors to this website and their physician.
Information reviewed by Dr. Rocío Parody Porras, Specialist in Haematology. Member of the Management of REDMO (Bone Marrow Donor Registry) and of the Foundation’s medical team. Barcelona Medical Association (Co. 35205)
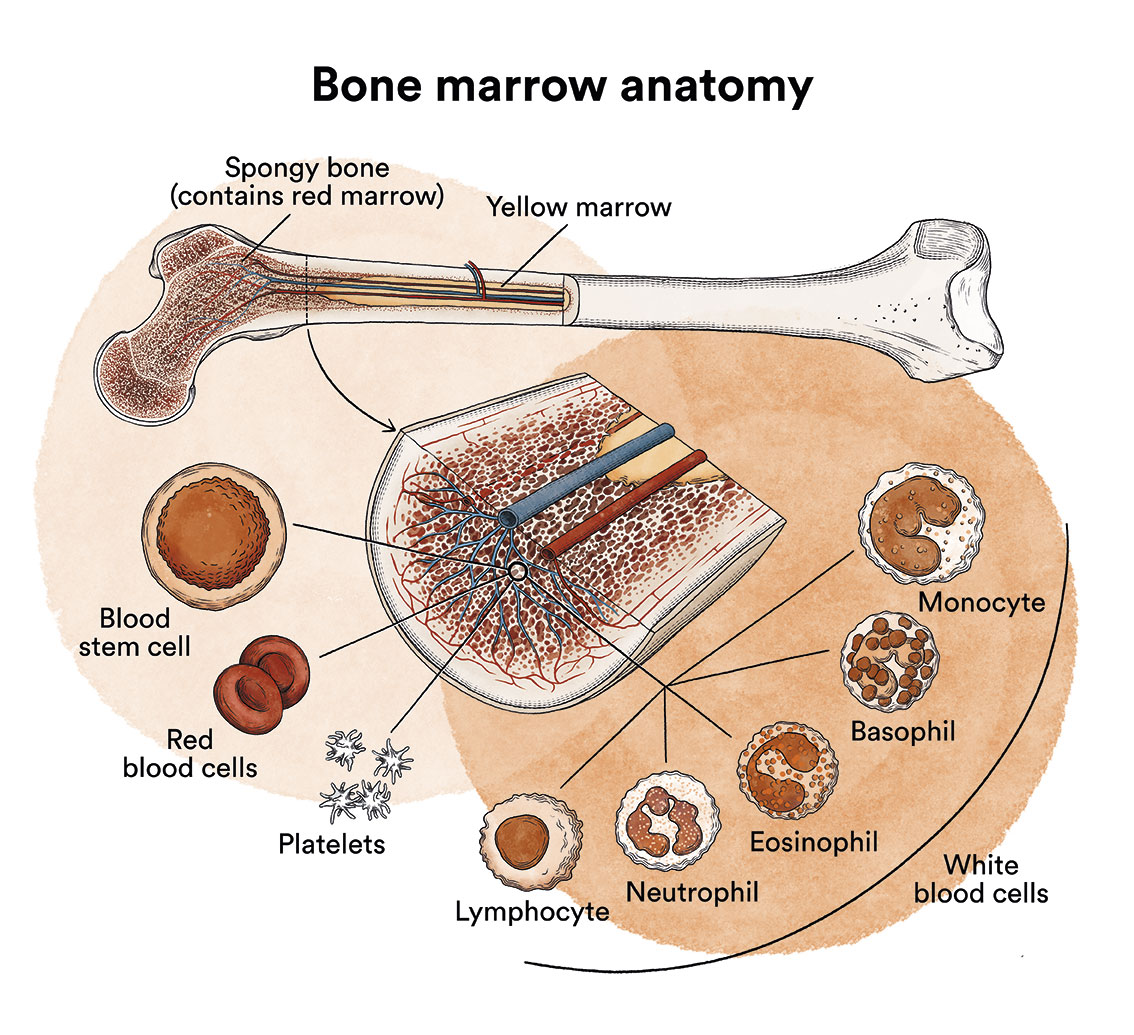
How does bone marrow work and what are the types of blood cells?
Polycythaemia vera is a type of blood cell cancer that originates in the bone marrow. See section Leukaemia, bone marrow and blood cells.
What is polycythaemia vera and who does it affect?
Polycythaemia is a malignant disease that falls into the group of chronic myeloproliferative neoplasms, along with primary myelofibrosis and essential thrombocythaemia, among others.
A common characteristic of these diseases is that the bone marrow stem cells, which are responsible for making all blood cells, have a defect that causes them to produce some of the myeloid blood cells in an uncontrolled manner.
In the case of polycythaemia vera, due to a mutation in a RBC-producing cell, the blood thickens due to a significant increase in red blood cells.
In our country, the incidence of polycythaemia vera is 4-6 cases per million inhabitants per year, with the median age of diagnosis being 60 years. This disease is rare before the age of 40.
We recommend reading the Educational guide on polycythaemia vera of the Spanish Group of Philadelphia Negative Chronic Myeloproliferative Diseases (GEMFIN) of the Spanish Society of Haematology and Haemotherapy (SEHH).
What are the causes of polycythaemia vera?
It is not known why polycythaemia vera occurs.
At the cytogenetic level, polycythaemia vera is caused by genetic mutations. These mutations alter the system that regulates the formation of blood cells, known as the JAK-STAT pathway. In people with polycythaemia vera, this pathway is permanently activated, i.e. it does not stop working at any time, causing the stem cells to keep multiplying and, moreover, to function in an altered way.
What are the symptoms of polycythaemia vera?
In most cases, it is a disease that has no symptoms and is therefore diagnosed by chance in a routine blood test. If clinical manifestations are present, they may be: non-specific symptoms (50% of cases) (asthaenia, night sweats, weight loss, gout attacks, epigastric discomfort, generalised pruritus [picores] ); thrombotic phenomena (50% of cases), cerebral vascular accidents, angina pectoris, heart attacks, intermittent claudication of the lower limbs and thrombosis of abdominal veins (portal, splenic, hepatic); peripheral vascular insufficiency (redness and pain/burning in the fingers and soles of the feet that worsen with heat (shower) and improve with exposure to cold. Haemorrhages (epistaxis, gingivorrhages, digestive bleeding) and neurological manifestations (60%) (headaches, tingling in hands and feet, vertiginous sensations, visual disturbances) are also not uncommon (15-30% of cases).
How is polycythaemia vera diagnosed?
It is not possible to confirm the diagnosis of polycythaemia vera with a blood test alone. Three measurements of red blood cell concentration can be used to diagnose polycythaemia vera: haematocrit (greater than 51% in men and 48% in women), haemoglobin concentration (greater than 185 g/l in men and 165 g/l in women) and red blood cell count (values exceeding 5-6 million). These measurements are included in a standard blood test, haemogram, so the diagnosis of suspected PV is relatively simple to establish. A haemogram also frequently shows increased white blood cell count (leukocytosis) and platelet count (thrombocytosis).
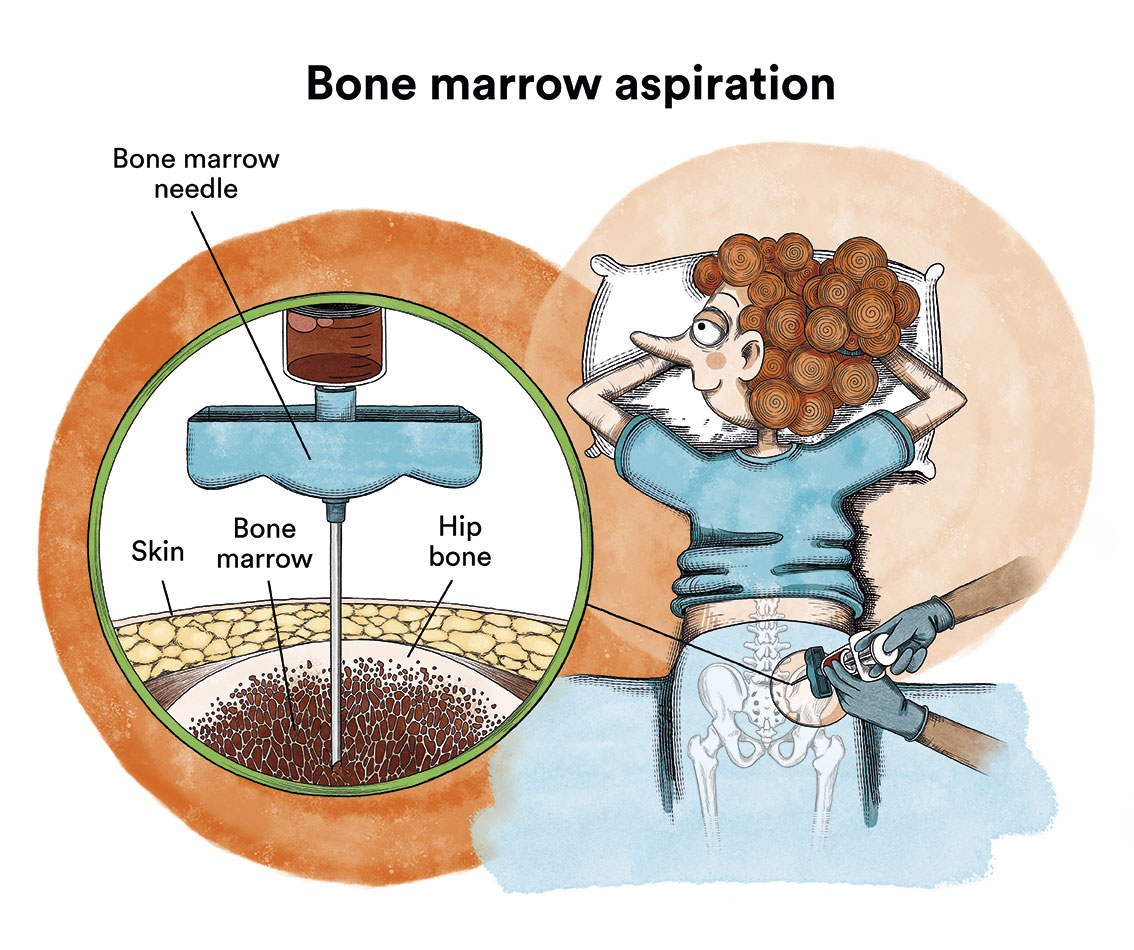
To complete the study and establish a definitive diagnosis, at least one molecular study (to detect the presence of a specific mutation of the JAK2 gene), a bone marrow biopsy and the quantification of serum erythropoietin (always low) must be carried out.
What is the treatment for polycythaemia vera?
 Treatment of polycythaemia vera should be based on therapeutic bloodletting, acetylsalicylic acid (ASA or aspirin), and hydroxyurea or radioactive phosphorus.
Treatment of polycythaemia vera should be based on therapeutic bloodletting, acetylsalicylic acid (ASA or aspirin), and hydroxyurea or radioactive phosphorus.
In low-risk patients (age < 60 years and no history of thrombosis), bloodletting is the treatment of choice in most cases. They are performed every 3 to 4 days and 400mL of blood is drawn to reduce the haematocrit (up to 45% in men or 42% in women). These are accompanied by regular monitoring of the patient.
In high-risk patients (based on age > 60 years or history of thrombosis) the treatment of choice is hydroxyurea. Alternatives include busulfan and radioactive phosphorus, especially in older patients, interferon alpha in younger patients, and in cases of resistance, ruxolitinib.
Unless contraindicated, all patients should receive 100 mg per day of acetylsalicylic acid. Many patients also require allopurinol to reduce uric acid levels.
In patients with significant thrombocytosis, anagrelide may be indicated.
What is the prognosis for patients with polycythaemia vera?
Although it is not a curable disease, its chronic nature means that it can be managed effectively over long periods of time. Despite this, the increased number of red blood cells and platelets in the blood can lead to the haemorrhagic and/or thrombotic complications mentioned above. Over the years, patients with PV may progress to myelofibrosis with marrow depletion (deficiency of all normal blood elements). Similarly, and especially after many years of treatment with hydroxyurea, progression to acute myeloblastic leukaemia may occur.
We advise polycythemia patients in Spain to contact MPN, the Spanish association of patients with chronic myeloproliferative neoplasms.
Links of interest concerning medical issues relating to polycythaemia vera
- An educational guide to polycythaemia vera. Spanish Group of Philadelphia Negative Chronic Myeloproliferative Diseases (GEMFIN) of the Spanish Society of Haematology and Haemotherapy (SEHH).
- Myeloproliferative neoplasms. Leukemia & Lymphoma Society
- Information on myeloproliferative syndromes. AEAL
- Treatment of neoplasms of chronic myeloproliferative neoplasms. National Cancer Institute
- Philadelphia Negative Chronic Proliferative Neoplasms Patient Recommendations Manual. Spanish Group of Philadelphia Negative Chronic Myeloproliferative Diseases (GEMFIN) of the Spanish Society of Haematology and Haemotherapy (SEHH).
Links of interest on other topics related to polycythaemia vera
TESTIMONIAL MATERIALS
You can order the booklets in paper format for free delivery in Spain by e-mail: imparables@fcarreras.es
BONE MARROW TRANSPLANT
- Bone Marrow Transplant Guide. Josep Carreras Foundation (content in Spanish)
- What is HLA and how does it work? Josep Carreras Foundation (content in Spanish)
- Graft-versus-Host Disease. Josep Carreras Foundation (content in Spanish)
- History of Bone Marrow Transplantation. Josep Carreras Foundation (content in Spanish)
- How is the search for an anonymous donor conducted? Josep Carreras Foundation (content in Spanish)
FOOD
- How to maintain a healthy diet during treatment? Josep Carreras Foundation (content in Spanish)
- Nutrition guide. Leukemia & Lymphoma Society
OTHER
- Ideas on what to take with me to the isolation chamber. Josep Carreras Leukaemia Foundation (content in Spanish)
- Travel tips for people with cancer. Josep Carreras Leukaemia Foundation (content in Spanish)
- Physiotherapy manual for haematological and transplant patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Prevention and treatment of oral mucositis. Josep Carreras Leukaemia Foundation (content in Spanish)
- Oral hygiene in oncohaematological patients. Josep Carreras Leukaemia Foundation (content in Spanish)
- Fertility manual: Suffering from blood cancer and becoming a parent. Josep Carreras Leukaemia Foundation (content in Spanish)
- Skin care in the oncohaematological patient. Josep Carreras Leukaemia Foundation (content in Spanish)
- Aesthetic Oncology Manual. Josep Carreras Leukaemia Foundation (content in Spanish)
- Leukaemia and sexuality. Josep Carreras Leukaemia Foundation (content in Spanish)
- 7 ways to wear a scarf. Josep Carreras Leukaemia Foundation (content in Spanish)
Links of interest: local/provincial or state entities that can provide you with resources and services specialised in leukaemia or cancer patients:
In Spain there is a large network of associations for haematological cancer patients that, in many cases, can inform you, advise you and even carry out certain procedures. These are the contacts of some of them by Autonomous Communities:
All these organisations are external to the Josep Carreras Foundation.
STATE
- MPN España (Asociación de Afectados Por Neoplasias Mieloproliferativas Crónicas)
- CEMMP (Comunidad Española de Pacientes de Mieloma Múltiple)
- AEAL (ASOCIACIÓN ESPAÑOLA DE AFECTADOS POR LINFOMA, MIELOMA y LEUCEMIA)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact with the nearest branch or call 900 100 036 (24h).
- AELCLES (Agrupación Española contra la Leucemia y Enfermedades de la Sangre)
- Josep Carreras Leukaemia Foundation
- FUNDACIÓN SANDRA IBARRA
- GEPAC (GRUPO ESPAÑOL DE PACIENTES CON CÁNCER)
ANDALUCÍA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ALUSVI (ASOCIACIÓN LUCHA Y SONRÍE POR LA VIDA). Sevilla
- APOLEU (ASOCIACIÓN DE APOYO A PACIENTES Y FAMILIARES DE LEUCEMIA). Cádiz
ARAGÓN
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASPHER (ASOCIACIÓN DE PACIENTES DE ENFERMEDADES HEMATOLÓGICAS RARAS DE ARAGÓN)
- DONA MÉDULA ARAGÓN
ASTURIAS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASTHEHA (ASOCIACIÓN DE TRASPLANTADOS HEMATOPOYÉTICOS Y ENFERMOS HEMATOLÓGICOS DE ASTURIAS)
CANTABRIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LA MANCHA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
CASTILLA LEÓN
- ABACES (ASOCIACIÓN BERCIANA DE AYUDA CONTRA LAS ENFERMEDADES DE LA SANGRE)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ALCLES (ASOCIACIÓN LEONESA CON LAS ENFERMEDADES DE LA SANGRE). León.
- ASCOL (ASOCIACIÓN CONTRA LA LEUCEMIA Y ENFERMEDADES DE LA SANGRE). Salamanca.
CATALUÑA
- ASSOCIACIÓ FÈNIX. Solsona
- FECEC (FEDERACIÓ CATALANA D’ENTITATS CONTRA EL CÁNCER
- FUNDACIÓ KÁLIDA. Barcelona
- FUNDACIÓ ROSES CONTRA EL CÀNCER. Roses
- LLIGA CONTRA EL CÀNCER COMARQUES DE TARRAGONA I TERRES DE L’EBRE. Tarragona
- MielomaCAT
- ONCOLLIGA BARCELONA. Barcelona
- ONCOLLIGA GIRONA. Girona
- ONCOLLIGA COMARQUES DE LLEIDA. Lleida
- ONCOVALLÈS. Vallès Oriental
- OSONA CONTRA EL CÀNCER. Osona
- SUPORT I COMPANYIA. Barcelona
- VILASSAR DE DALT CONTRA EL CÀNCER. Vilassar de Dalt
VALENCIAN COMMUNITY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASLEUVAL (ASOCIACIÓN DE PACIENTES DE LEUCEMIA, LINFOMA, MIELOMA Y OTRAS ENFERMEDADES DE LA SANGRE DE VALENCIA)
EXTREMADURA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- AFAL (AYUDA A FAMILIAS AFECTADAS DE LEUCEMIAS, LINFOMAS; MIELOMAS Y APLASIAS)
- AOEX (ASOCIACIÓN ONCOLÓGICA EXTREMEÑA)
GALICIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- ASOTRAME (ASOCIACIÓN GALLEGA DE AFECTADOS POR TRASPLANTES MEDULARES)
BALEARIC ISLANDS
- ADAA (ASSOCIACIÓ D’AJUDA A L’ACOMPANYAMENT DEL MALALT DE LES ILLES BALEARS)
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
CANARY ISLANDS
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- AFOL (ASOCIACIÓN DE FAMILIAS ONCOHEMATOLÓGICAS DE LANZAROTE)
- FUNDACIÓN ALEJANDRO DA SILVA
LA RIOJA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
MADRID
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- AEAL (ASOCIACIÓN ESPAÑOLA DE LEUCEMIA Y LINFOMA)
- CRIS CONTRA EL CÁNCER
- FUNDACIÓN LEUCEMIA Y LINFOMA
MURCIA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
NAVARRA
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
BASQUE COUNTRY
- AECC (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER). Present is the different provinces and in many municipalities. Contact the nearest branch.
- PAUSOZ-PAUSO. Bilbao
AUTONOMOUS CITIES OF CEUTA AND MELILLA
- AECC CEUTA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
- AECC MELILLA (ASOCIACIÓN ESPAÑOLA CONTRA EL CÁNCER)
Support and assistance
We also invite you to follow us through our main social media (Facebook, Twitter and Instagram) where we often share testimonies of overcoming this disease.
If you live in Spain, you can also contact us by sending an e-mail to imparables@fcarreras.es so that we can help you get in touch with other people who have overcome this disease.

* In accordance with Law 34/2002 on Information Society Services and Electronic Commerce (LSSICE), the Josep Carreras Leukemia Foundation informs that all medical information available on www.fcarreras.org has been reviewed and accredited by Dr. Enric Carreras Pons, Member No. 9438, Barcelona, Doctor in Medicine and Surgery, Specialist in Internal Medicine, Specialist in Hematology and Hemotherapy and Senior Consultant of the Foundation; and by Dr. Rocío Parody Porras, Member No. 35205, Barcelona, Doctor in Medicine and Surgery, Specialist in Hematology and Hemotherapy and attached to the Medical Directorate of the Registry of Bone Marrow Donors (REDMO) of the Foundation).
Become a member of the cure for leukaemia!


